What is Foraminal Stenosis?
Foraminal stenosis is a ‘pain the back’ that, if left undiagnosed and untreated, can become a very serious condition. Here is what you need to know about foraminal stenosis.
“Foraminal stenosis is when the foramen is constricted and compressed against the spinal cord and/or spinal nerves,” reports Spines.Com. “The foramen is the opening between the spinal vertebrae and spinal nerve exits.”
The condition known as foraminal stenosis involves the narrowing of the patient’s spinal foramen. This is the hole a spinal nerve passes as it exits the spine. Foraminal stenosis also is defined as the narrowing of the cervical disc space. Foraminal stenosis is a form of spinal stenosis (otherwise known as cervical spinal stenosis). This condition–according to The American Academy of Orthopedic Surgeons–afflicts 8-11 percent of the population. Other sources report a higher percentage, with Healthline stating that nearly 50 percent of middle-aged people and senior citizens suffer from stenosis or pinched nerves.
Commonly referred to as baby boomer back, spinal stenosis disproportionately affects people over 50. Even teenagers can develop this condition, which develops over time. The condition involves the narrowing of the spinal canal. The variety and name of the stenosis condition will depend on the location of the illness.
Foraminal stenosis can affect the entire spine. This is because individual foramen can be found at every level of the spine, with one resting on each side. At each level of the spine, a spinal nerve–one coming to or from the spinal cord–passes through a foramen. And as the foramen is a small body part, anything that touches that region can lead to foraminal stenosis.
It is an enlargement of the joint, and the sensitivity and delicacy of a nerve root on one side, that causes foraminal stenosis. Yet before we go on, it is important to remember the role that the spinal column plays in the life, body, and health of a human being.
Foraminal stenosis is one of many serious conditions that affects the spinal column; a nerve center that runs all the way from the base of the brain to the backbone, including the vertebral canal. The brain and spine together form the central nervous system.
The spinal column supports the whole body, empowering us to stand, twist and bend. The spinal column shields the spinal cord from harm and injury. A spinal condition could rob the body of strength, feeling, and those functions that enable us to live, work and spend quality time with our friends and families each day.
The functions of the spinal cord include electrical communication, walking ability, involuntary reflexes, and other vital bodily purposes and activities.
Any harm to the spine can impact the patient’s life. This is particularly true of foraminal stenosis. Spinal stenosis is also referred to as pinched nerves. Whenever a foreign object pressures the spinal nerves, then pinched nerves can result.
Foraminal Stenosis Causes
Foraminal stenosis causes can differ as much as the condition’s effects. Most instances can be traced to a single cause. Advanced age is the root of most foraminal stenosis cases. As people age, and as their bodies undergo both normal and vigorous physical activity, their spinal column degenerates. And those who–due to work, sports, or other physical activity–perform more physical activity than others, are more prone to develop foraminal stenosis and other degenerative spine diseases.
This can happen to the healthiest, most active of older adults. And if the patient is dealing with other orthopedic health conditions, such as bulging discs, herniated discs (in which the intervertebral discs that cushion each of the spine’s vertebral spine bone protrude), bony growths or spurs (in which the cartilage roughens or wears, permitting bones to rub against each other until small bone spurs or growths develop), and soft tissue swelling. Various intrusive growths and tissues can impact the foramen–exerting pressure on the spinal nerves.
Osteoarthritis, a condition in which the spine’s cushioning cartilage degenerates with age, is the most major and frequent cause of foraminal stenosis. Also known as spondylosis, spinal osteoarthritis is painful and life-impairing. A degenerative condition that can affect any spinal region, osteoarthritis can impair the spine’s intervertebral discs and facet joints–reducing the space between vertebral discs and limiting the patient’s movement. This leads to related conditions such as bone spurs and foraminal stenosis.
This spinal disorder happens as the direct effect of other orthopedic conditions. The seriousness of the condition will depend on the number of foramine affected.
Foraminal Stenosis Symptoms
Foraminal stenosis symptoms can be attributed to other causes and sources. Stenosis can be primary or congenital, meaning that the condition was inherited at birth. Foraminal stenosis symptoms may not show up until the patient’s middle-aged or advanced years. Sometimes the disease can be attributed to spondylolisthesis, tumors or cysts, a bone disease such as Paget’s disease, and genetic conditions like dwarfism.
Foraminal stenosis can be diagnosed through symptoms that–while serious and painful–tend to vary. This is because the foramen is found on each individual level of the spinal column. The foramen pinches one or more nerves. The location of the pinched nerve or nerves determines the specific symptoms.
Every single foramen encloses one nerve that travels to a specific body part. A foramen on the right side of the body will contain a nerve that travels to that side.
This case of foraminal stenosis will occur on the right side of the body–affecting the motor and sensory function in that area.
When foramen disease strikes the spine’s lower region, it is likely to affect the leg. When the foramen is located in the neck or the cervical area, the arm is more likely to suffer.
An exception to this rule happens when foramen on both sides of a particular nerve have been harmed or impacted.
Regardless of the location of the foraminal stenosis condition, the symptoms can be similar in many cases. Patients can experience numbness and tingling, along with either dull or sharp pain and burning sensations. Motor symptoms include weakness, reflex problems, and that prickly, tingly sensation described as the ‘pins and needles’ feeling. Most people have experienced the pins and needles feeling, when their leg ‘falls asleep’ after a period of rest or idleness. Yet if this sensation strikes more frequently than usual, and on one side of the body, then you may have foraminal stenosis. The condition can result in loss of function, with some patients suffering a loss of feeling and/or movement.
People suffering from foraminal stenosis may have difficulty walking or even standing up straight. In severe and extreme cases, foraminal stenosis can result in paralysis.
Yes, even paralysis can occur due to foraminal stenosis. And, as happens with this serious orthopedic disorder, any paralysis will strike only one side of the body. The specific muscles immobilized are those controlled by the nerve being pinched.
Not every case of foraminal stenosis will result in even temporary paralysis. This symptom is most likely to occur if the foraminal stenosis is undiagnosed and/or untreated. If this condition is ignored or not detected, then afflicted nerves may die, which can lead to loss of bodily function.
Lumbar Foraminal Stenosis
Foraminal stenosis is often referred to as Lumbar Foraminal Stenosis. This is because the condition of foraminal stenosis most commonly strikes the lumbar or lower back section of the spine.
Foraminal stenosis can be a difficult condition to diagnose, both because of the different locations of its symptoms, and the similarity of these telltale signs to other orthopedic conditions. Some of these symptoms can come about because of conditions that don’t involve the spine. This is why, if you regularly experience the symptoms of foraminal stenosis, it is important that you consult an orthopedic physician. This doctor will administer MRI scans of the spine. These are the ideal imaging tests to examine small and subtle areas of the spine that include the foramen.
Foraminal Stenosis C5-C6 Condition
Aside from diagnosing foraminal stenosis, the MRI may determine the location and classification of this condition in the patient’s body. In the condition classification known as foraminal stenosis c5-c6, the disorder strikes the C5-C6 vertebrae along with the disc situated between them. Situated beneath the center of the cervical spine, this spinal section supplies the neck with structural support and flexibility.
Foraminal Stenosis I5 S1 Condition
Another common instance of foraminal stenosis, foraminal stenosis l5 s1, afflicts the L5 and S1 vertebrae in the lower spine. This is where the nerve roots branch away from the spinal cord and down the legs. These vertebrae mark the site where the last vertebra of the lumbar spine (l5) meets the sacrum’s top; creating a junction called the lumbosacral joint.
Once foraminal stenosis is diagnosed, then the patient’s next logical question will be, “what is the treatment for severe foraminal stenosis?” This will be true regardless of the condition’s severity. Any condition of foraminal stenosis can limit the everyday activities and life of the patient.
Foraminal Stenosis Treatment
Luckily for patients and their families, many foraminal stenosis treatment options are available. The options that the physician and patient team pursue will depend on the severity and degree of the foraminal stenosis condition.
The good news is that relatively mild foraminal stenosis can be treated via a brief regimen of rest. Avoid vigorous or strenuous activity and take it easy for a few days. This may rest and repair pinched nerves, however–like the trauma that may have caused the condition–it is important not to give up all activity for too long. Your body needs regular exercise in order to thrive.
Light exercise and stretching might loosen pinched nerves and stabilize your spine–enhancing one’s range of motion and opening more space through which the nerves can pass. Certain stretches–including the sitting spinal stretch, the standing hamstring stretch, the knee to opposite soldier, etc.–can, when performed under the supervision of a doctor or certified personal trainer, ease the effects of foraminal stenosis.
Hot and cold treatments can be useful in treating this condition. Apply cold packs to the afflicted region for several days, then switch off to warm packs or heating pads. Cold pads soothe and numb the pain of foraminal stenosis.
For more severe cases of foraminal stenosis, more intensive treatments might be prescribed. NSAIDs such as aspirin, or steroids such as prednisone, might be recommended. A change in diet might be suggested, as weight loss can take pressure from the spine and nerve roots. And the physician might briefly apply a neck brace or soft cervical collar. This move will restrict your movement and relax your neck muscles.
Foraminal Stenosis Surgery
If these methods of treating foraminal stenosis prove unsuccessful, then the physician/patient team might explore the option of foraminal stenosis surgery. Although no one likes to consider surgery, especially in a sensitive area such as the spine, today’s medical technology offers high tech, minimally invasive surgical procedures to treat and resolve foraminal stenosis.
Probably the most common form of foraminal stenosis surgery is a Foraminotomy. In this procedure, the afflicted nerve is decompressed. The surgeon removes the bone and tissue overlying the foramen. This procedure opens the foramen, thus allowing the nerve more room to pass and move. This minimally invasive surgery can be conducted through a small incision.
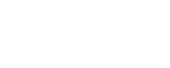
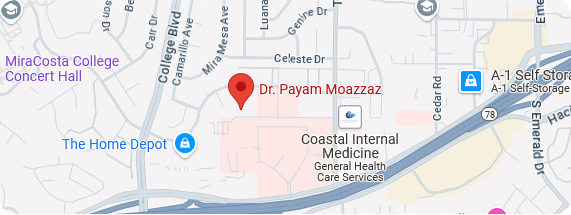
To explore these options and others, consult Dr. Payam Moazzaz regarding your foraminal stenosis condition.
Dr. Payam Moazzaz has a decade’s worth of experience in the orthopedic field, and has achieved milestones in the exciting field of minimally invasive surgery and its innovative subset, robotic spine surgery. He ranks among the first surgeons to perform robotic spine surgery via a first-generation platform that earned FDA approval in 2011. He is among the first physicians to use a robotic spine surgery platform called Mazor X, which was introduced on a national level in 2016. Dr. Moazzaz has performed more than 500 spine surgeries using robotic technology, the most robotic spine surgeries in the State of California. Moreover, Dr. Moazzaz is the only California physician to achieve a perfect, 100 percent record of successful surgeries.
Using the latest in high tech medical technology, robotic surgery involves advanced imagery to eliminate the muss and fuss of traditional surgery. To use the most technologically advanced terms possible.
The process of this spinal surgery begins several days before the procedure, when images are taken of the patient to generate a three-dimensional image of the spine. This image will be used as a blueprint for the foraminal stenosis surgery, pinpointing the specific areas that require the surgeon’s attention; in this instance, the afflicted foramen of the spinal column.
This advanced, minimally invasive form of foraminal stenosis surgery saves the patient from excessive poking and prodding. Armed with detailed three-dimensional images, the surgeon inserts miniature surgical instruments through smaller incisions via robotic arms. This gives the surgeon unlimited motion and precision.
A high-definition, three-dimensional camera directs the surgeon through the surgical procedure by way of a computerized monitor and console. By accessing this interior view of the patient’s back, the surgeon performs each move of the surgery with the aid of their robotic counterpart.
The advanced technology of robotic science has revolutionized foraminal stenosis surgery, and minimizes foraminal stenosis surgery risks. This brand of spinal fusion surgery is a less painful surgical procedure involving a smaller quantity of blood loss, fewer complications, and a faster return to regular activities via a shorter foraminal stenosis surgery recovery time.
This variety of foraminal stenosis surgery results in reduced instances of infection, along with less overall damage to skin, muscles and tissue. These factors ensure a shorter surgery recovery time, a shorter hospital stay, and (if all goes well) a guarantee that your experience after foraminal stenosis surgery is more comfortable. You will make a smoother, faster return to work, family, and social/recreational activities.
The condition of foraminal stenosis can cause pain and discomfort, hindering both your daily activities and your life. Yet thanks to modern technology and the expertise of physicians like Dr. Payam Moazzaz, you can recover from most instances of foraminal stenosis. You soon will return in full to an active, successful existence. Contact New Era Spine today to arrange a consultation with Dr. Payam Moazzaz on the subject of spinal contusions.